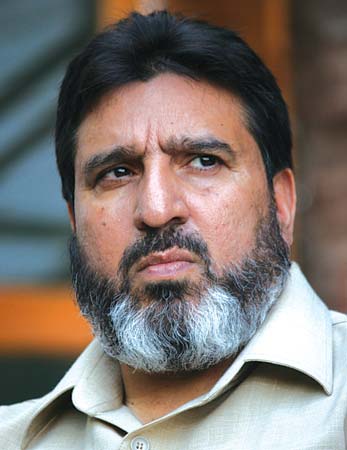
SRINAGAR: Secretary Health and Medical Education Department Bhupinder Kumar on Saturday termed the allegation of Rs 500 Cr loss to the exchequer regarding PMJAY SEHAT Scheme as baseless and far from reality.
Addressing a press conference in Jammu, Kumar said, “There is an allegation of losses to the exchequer to the tune of Rs 500 crores but a total of premium that was paid to the Bajaj Allianz during the whole policy period that began on April 26l 2020 and continued till March 2022 including the interim period of 79 days on stop loss basis, was Rs 304 crores.”
“Total premium that was paid to Bajaj was Rs 304 crores and during same period of one year and 79 days the claims pay out to both private and public by the insurance company was Rs 398.41 crores,” he said. “Based on these figures, the allegation of scam of Rs 500 crore is baseless. The fact is that the company instead of earning profit has on the contrary incurred monetary loss of Rs 93.2 crores.”
The Secretary health added that there has also been an attempt to build a false narrative on the baseless and wrong facts reported in some media outlets about the termination clause.
“It has also been alleged that the review of the renewal of contract was to be done after two years, however, it is being clarified that as per the contract between Bajaj allianz and State Health Agency J&K was allotted to Bajaj after competitive bidding process using the model tender document issued by the National Health Authority,” he said.
He said: “The maximum term of the contract was fixed three years which was to be renewed after every 12 months. The revision of clauses 9 and 27 of the contract make it clear that the continuation of the contract beyond the first year was to be on the basis of mutual agreement of both the parties.”
Kumar said that the insurance company as per the terms and conditions of the contract served the notice expressing unwillingness to continue the contract beyond the completion of one year in view of the losses incurred by it.
He said that every effort was made by the department at that time for ensuring continuing of the contract and services but the company chose to exercise the option of exiting after the expiry of one year term.
“To prevent service interruptions, State Health Agency J&K entered into an agreement with Bajaj alliance to continue services on stop loss basis until the selection of new insurance company is finalised,” he said, adding that it has also been misquoted that the number of eligible families covered under the scheme was increased by 10 lakhs to benefit the company during the interim period of 79 days but it is clarified that number of families during the policy period from 26th of January 2020 to 25th of December 2021 and the interim period of 79 days remained same as 21.24 lakhs.
He said that this model hasn’t only strengthened the health care systems within J&K but has also significantly reduced out of pocket expenses preventing catastrophic payments and poverty for families in need of hospitalization.
“However, it is worth mentioning that there have been attempts to discredit the scheme through misinformation. Such allegations are intended to disrupt the services and are totally baseless and false besides meant to malign the image of government and are vehemently denied,” he said.
Meanwhile, an official spokesman in a statement to KNO said that, the Secretary Health and Medical Education, Bhupinder Kumar has addressed concerns and allegations surrounding the implementation of the Pradhan Mantri Jan Arogya Yojana – SEHAT (PMJAY-SEHAT) scheme. “One of the key allegations was related to a loss of Rs. 500 Crores. The government clarified that the total premium paid to Bajaj Allianz General Insurance Company (BAGIC) during the policy period from December 26, 2020, to March 14, 2022, was Rs. 304.59 Crores, while the total claims payout to hospitals (both public and private) by BAGIC was Rs. 398.41 Crores. Consequently, the allegation of a loss is unsubstantiated as the insurance company incurred a monetary loss of Rs. 93.82 Crores,” the statement said.
The official statement said that Misinformation about the termination clause and contract renewal has also surfaced. According to the contract between BAGIC and the State Health Agency, the maximum term was fixed for three years and renewable every 12 months. “The continuation of the contract beyond the first year was to be based on mutual agreement, and the insurance company decided to exit after the first year due to incurred losses,” it said, adding that “To avoid service interruption, the State Health Agency of J&K entered into an interim arrangement with BAGIC on a Stop Loss basis until a new insurance company was selected. During this period, the government bore the entire risk of loss of claims. The arrangement was cost-effective and served the public interest by ensuring the continuity of healthcare services.”
The statement said that contrary to allegations that the number of eligible families was increased to benefit the insurance company, the government clarified that the number of families remained the same during the policy period, from December 26, 2020, to December 25, 2021, and the subsequent interim period of 79 days, totaling 21.24 lakhs.
“The Government of Jammu and Kashmir emphasized its adherence to the guidelines of the National Health Authority (NHA), Government of India, for the scheme’s implementation. This includes the use of the Model Tender Document for the transparent selection of insurance companies and the adoption of Health Benefits Packages (2.2 version) for implementation,” the statement said, adding that “since the launch of the PMJAY-SEHAT scheme, the government has paid Rs. 1175.32 Crores in premiums to insurance companies. In return, insurance companies disbursed a total of Rs. 1,249.33 Crores in claims to empaneled hospitals, benefiting approximately 5.67 lakh patients. The scheme has provided crucial medical care for patients with life-consuming and life-threatening diseases.”
The statement said that the insurance model has shifted the risk to insurance companies, leading them to pay nearly Rs. 74 Crores beyond the premium to empaneled public and private hospitals. This model has strengthened the healthcare system within the UT and significantly reduced out-of-pocket expenses for families in need of hospitalization.
“Additionally, a feedback system using QR codes and a 104 Call Centre has been implemented, with nearly 99% of patients rating their treatment experience as Excellent or Good,” the statement said, adding that “the government emphasized that allegations intended to discredit the scheme are baseless, false, and aimed at maligning its image. It reiterated its commitment to providing quality healthcare services to the public”—(KNO)