SRINAGAR: With nearly 3200 deaths and the evasive Coronavirus (Covid-19) spread to 44 countries since the year-end, the mass morbidity has impacted the economies and the fear is looming large across the world. Fresh cases have been reported from America where, in one particular case, the patient has no China travel or interaction history. In Hong Kong, even a dog has been tested positive for the virus.

Biological experts especially the virologists are working round the clock to get some intervention that will help halt its spread. There are almost score vaccines undergoing clinical trials but nothing is really available as part of the treatment.
Countries have closed borders. Iran did not had Friday congregations last week. Saudi Arabia has closed entry for all Umrah pilgrims from every country that has any reported case of the Coronavirus. In parts of Pakistan, schools have been closed. Almost every country is busy to protect its population but the virus has been reported from 44 countries even in cases where there is no China history.
World Health Organisation (WHO) that is the global leader in guiding in the management of epidemics had sent a team of 25 experts to Wuhan to study the crisis. It released its report on Friday. Titled Report of the WHO-China Joint Mission on Coronavirus Disease 2019, the report is vital in understanding the mess that the virus has created, its pathology and its infection mechanism. The 25 national and international experts from China, Germany, Japan, Korea, Nigeria, Russia, Singapore, the United States of America and the World Health Organization (WHO) were led by Dr Bruce Aylward (WHO) and Dr Wannian Liang of China.
Dr Tedros Adhanom, Director General WHO said the report carries “wealth of information”. He said: “It calls for all countries to educate their populations, to expand surveillance, to find, isolate and care for every case, to trace every contact, and to take an all-of-government and all-of-society approach – this is not a job for the health ministry alone.” He said the work is progressing on vaccines and therapeutics. “More than 20 vaccines are in development globally, and several therapeutics are in clinical trials. We expect the first results in a few weeks,” he said.
Here we are reproducing select passages of the report to help the people, doctors and the health system managers to understand from China.
The virus
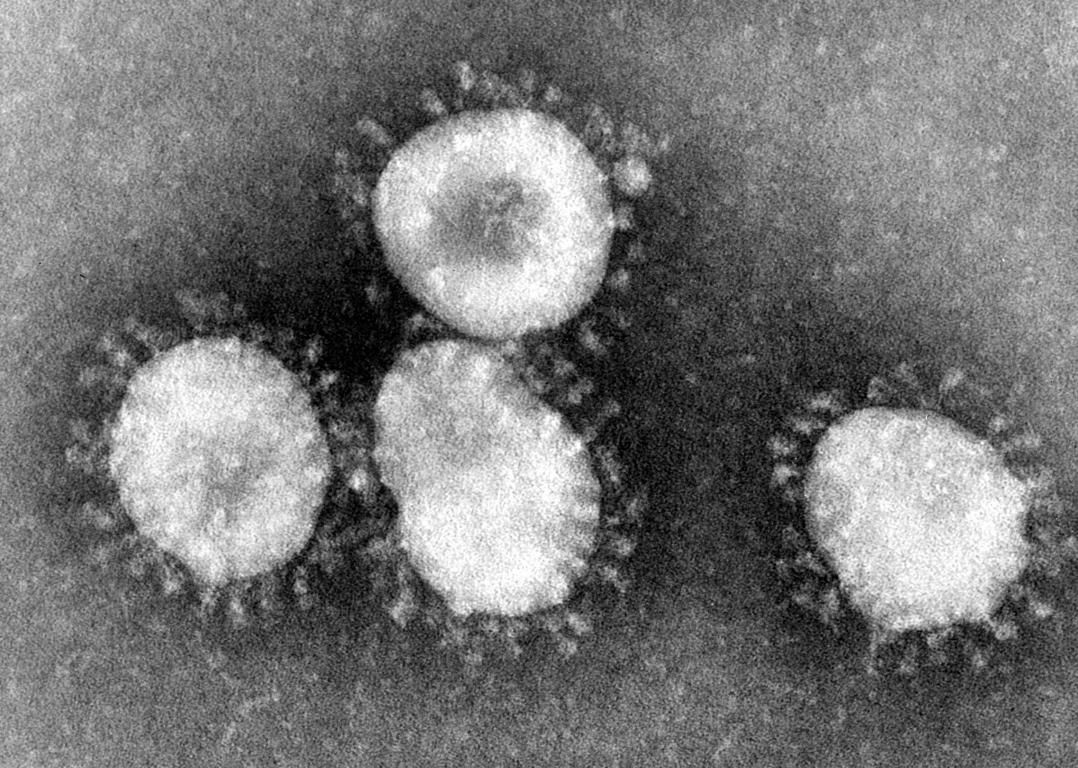
On 30 December 2019, three bronchoalveolar lavage samples were collected from a patient with pneumonia of unknown etiology – a surveillance definition established following the SARS outbreak of 2002-2003 – in Wuhan Jinyintan Hospital. Real-time PCR (RT-PCR) assays on these samples were positive for pan-Betacoronavirus. Using Illumina and nanopore sequencing, the whole genome sequences of the virus were acquired. Bioinformatic analyses indicated that the virus had features typical of the coronavirus family and belonged to the Betacoronavirus 2B lineage. Alignment of the full-length genome sequence of the COVID-19 virus and other available genomes of Betacoronavirus showed the closest relationship was with the bat SARS-like coronavirus strain BatCov RaTG13, identity 96%.
Virus isolation was conducted with various cell lines, such as human airway epithelial cells, Vero E6, and Huh-7. Cytopathic effects (CPE) were observed 96 hours after inoculation.
Typical crown-like particles were observed under a transmission electron microscope (TEM) with negative staining. The cellular infectivity of the isolated viruses could be completely neutralized by the sera collected from convalescent patients. Transgenic human ACE2 mice and Rhesus monkey intranasally challenged by this virus isolate induced multifocal pneumonia with interstitial hyperplasia. The COVID-19 virus was subsequently detected and isolated in the lung and intestinal tissues of the challenged animals.
Whole genome sequencing analysis of 104 strains of the COVID-19 virus isolated from patients in different localities with symptom onset between the end of December 2019 and mid-February 2020 showed 99.9% homology, without significant mutation.
Post-mortem samples from a 50-year old male patient from Wuhan were taken from the lung, liver, and heart. Histological examination showed bilateral diffuse alveolar damage with cellular fibromyxoid exudates. The lung showed evident desquamation of pneumocytes and hyaline membrane formation, indicating acute respiratory distress syndrome (ARDS). Lung tissue also displayed cellular and fibromyxoid exudation, desquamation of pneumocytes and pulmonary oedema. Interstitial mononuclear inflammatory infiltrates, dominated by lymphocytes, were seen in both lungs.
Multinucleated syncytial cells with atypical enlarged pneumocytes characterized by large nuclei, amphophilic granular cytoplasm, and prominent nucleoli were identified in the intraalveolar spaces, showing viral cytopathic-like changes. No obvious intranuclear or intracytoplasmic viral inclusions were identified.
The Outbreak
As of 20 February 2020, a cumulative total of 75, 465 COVID-19 cases were reported in China. Reported cases are based on the National Reporting System (NRS) between the National and Provincial Health Commissions. The NRS issues daily reports of newly recorded confirmed cases, deaths, suspected cases, and contacts. A daily report is provided by each province at 0300hr in which they report cases from the previous day.

The NRS issues daily reports of newly recorded confirmed cases, deaths, suspected cases, and contacts. A daily report is provided by each province at 0300hr in which they report cases from the previous day.
…
Based on these epidemic curves, the published literature, and our on-site visits in Wuhan (Hubei), Guangdong (Shenzhen and Guangzhou), Sichuan (Chengdu), and Beijing, the Joint Mission team has made the following epidemiological observations:
Among 55,924 laboratory-confirmed cases reported as of 20 February 2020, the median age is 51 years (range 2 days-100 years old; IQR 39-63 years old) with the majority of cases (77.8%) aged between 30–69 years. Among reported cases, 51.1% are male, 77.0% are from Hubei and 21.6% are farmers or laborers by occupation.
Zoonotic Origins
COVID-19 is a zoonotic virus. From phylogenetics analyses undertaken with available full genome sequences, bats appear to be the reservoir of COVID-19 virus, but the intermediate host(s) has not yet been identified. However, three important areas of work are already underway in China to inform our understanding of the zoonotic origin of this outbreak.
These include early investigations of cases with symptom onset in Wuhan throughout December 2019, environmental sampling from the Huanan Wholesale Seafood Market and other area markets, and the collection of detailed records on the source and type of wildlife species sold at the Huanan market and the destination of those animals after the market was closed.
Routes of transmission
COVID-19 is transmitted via droplets and fomites during close unprotected contact between an infector and infectee. The airborne spread has not been reported for COVID-19 and it is not believed to be a major driver of transmission based on available evidence; however, it can be envisaged if certain aerosol-generating procedures are conducted in health care facilities.
Faecal shedding has been demonstrated by some patients, and the viable virus has been identified in a limited number of case reports. However, the faecal-oral route does not appear to be a driver of COVID-19 transmission; its role and significance for COVID-19 remain to be determined.
Household transmission
In China, human-to-human transmission of the COVID-19 virus is largely occurring in families. The Joint Mission received detailed information from the investigation of clusters and some household transmission studies, which are ongoing in a number of Provinces.
Among 344 clusters involving 1308 cases (out of a total of 1836 cases reported) in Guangdong Province and Sichuan Province, most clusters (78%-85%) have occurred in families. Household transmission studies are currently underway, but preliminary studies ongoing in Guangdong estimate the secondary attack rate in households ranges from 3-10%.
Contact Tracing
China has a policy of meticulous case and contact identification for COVID-19. For example, in Wuhan, more than 1800 teams of epidemiologists, with a minimum of 5 people/team, are tracing tens of thousands of contacts a day. Contact follow up is painstaking, with a high percentage of identified close contacts completing medical observation. Between 1% and 5% of contacts were subsequently laboratory-confirmed cases of COVID-19, depending on location.
For example: As of 17 February, in Shenzhen City, among 2842 identified close contacts, 2842 (100%) were traced and 2240 (72%) have completed medical observation. Among the close contacts, 88 (2.8%) were found to be infected with COVID-19.

As of 17 February, in Sichuan Province, among 25493 identified close contacts, 25347 (99%) were traced and 23178 (91%) have completed medical observation. Among the close contacts, 0.9% were found to be infected with COVID-19.
As of 20 February, in Guangdong Province, among 9939 identified close contacts, 9939 (100%) were traced and 7765 (78%) have completed medical observation. Among the close contacts, 479 (4.8%) were found to be infected with COVID-19.
Testing
The Joint Mission systematically enquired about testing for COVID-19 from routine respiratory disease surveillance systems to explore if COVID-19 is circulating more broadly and undetected in the community in China. These systems could include RT-PCR testing of COVID-19 virus in influenza-like-illness (ILI) and severe acute respiratory infection (SARI) surveillance systems, as well as testing of results among all visitors to fever clinics.
In Wuhan, COVID-19 testing of ILI samples (20 per week) in November and December 2019 and in the first two weeks of January 2020 found no positive results in the 2019 samples, 1 adult positive in the first week of January, and 3 adults positive in the second week of January; all children tested were negative for COVID-19 although a number were positive for influenza. In Guangdong, from 1-14 January, only 1 of more than 15000 ILI/SARI samples tested positive for the COVID-19 virus. In one hospital in Beijing, there were no COVID-19 positive samples among 1910 collected from 28 January 2019 to 13 February 2020. In a hospital in Shenzhen, 0/40 ILI samples were positive for COVID-19.
Within the fever clinics in Guangdong, the percentage of samples that tested positive for the COVID-19 virus has decreased over time from a peak of 0.47% positive on 30 January to 0.02% on 16 February. Overall in Guangdong, 0.14% of approximately 320,000 fever clinic screenings were positive for COVID-19.
Susceptibility
As COVID-19 is a newly identified pathogen, there is no known pre-existing immunity in humans. Based on the epidemiologic characteristics observed so far in China, everyone is assumed to be susceptible, although there may be risk factors increase susceptibility to infection. This requires further study, as well as to know whether there is neutralising immunity after infection.
The Transmission Dynamics
It is important to note that the transmission dynamics of an outbreak are inherently contextual. For COVID-19, we observe four major types of transmission dynamics during the epidemic growth phase and in the post-control period, and highlight what is known about transmission in children, as follows:
In Wuhan
Early cases identified in Wuhan are believed to be have acquired infection from a zoonotic source as many reported visiting or working in the Huanan Wholesale Seafood Market. As of 25 February, an animal source has not yet been identified.
At some point early in the outbreak, some cases generated human-to-human transmission chains that seeded the subsequent community outbreak prior to the implementation of the comprehensive control measures that were rolled out in Wuhan. The dynamics likely approximated mass action and radiated from Wuhan to other parts of Hubei province and China, which explains a relatively high R0 of 2-2.5.
The cordon sanitaire around Wuhan and neighbouring municipalities imposed since 23 January 2020 has effectively prevented further exportation of infected individuals to the rest of the country.
In Hubei
In the prefectures immediately adjoining Wuhan (Xiaogan, Huanggang, Jingzhou and Ezhou), the transmission is less intense. For other prefectures, due to fewer transport links and human mobility flows with Wuhan, the dynamics are more closely aligned with those observed in the other areas of the country. Within Hubei, the implementation of control measures (including social distancing) has reduced the community force of infection, resulting in the progressively lower incident reported case counts.
Outside Hubei
Given Wuhan’s transport hub status and population movement during the Chinese New Year (chunyun), infected individuals quickly spread throughout the country, and were particularly concentrated in cities with the highest volume of traffic with Wuhan. Some of these imported seeds generated limited human-to-human transmission chains at their destination.
Given the Wuhan/Hubei experience, a comprehensive set of interventions, including aggressive case and contact identification, isolation and management and extreme social distancing, have been implemented to interrupt the chains of transmission nationwide. To date, most of the recorded cases were imported from or had direct links to Wuhan/Hubei.
Community transmission has been very limited. Most locally generated cases have been clustered, the majority of which have occurred in households, as summarized above.
Of note, the highly clustered nature of local transmission may explain a relatively high R0 (22.5) in the absence of interventions and low confirmed case counts with intense quarantine and social distancing measures.
Special Settings
We note that instances of transmission have occurred within health care settings prisons and other closed settings. At the present time, it is not clear what role these settings and groups play in transmission. However, they do not appear to be major drivers of the overall epidemic dynamics. Specifically, we note:
A: Transmission in health care settings and among health care workers (HCW): The Joint Mission discussed nosocomial infection in all locations visited during the Mission. As of 20 February 2020, there were 2,055 COVID-19 laboratory-confirmed cases reported among HCW from 476 hospitals across China. The majority of HCW cases (88%) were reported from Hubei.
Remarkably, more than 40,000 HCW have been deployed from other areas of China to support the response in Wuhan. Notwithstanding discrete and limited instances of nosocomial outbreaks (e.g. a nosocomial outbreak involving 15 HCW in Wuhan), transmission within health care settings and amongst health care workers does not appear to be a major transmission feature of COVID-19 in China. The Joint Mission learned that, among the HCW infections, most were identified early in the outbreak in Wuhan when supplies and experience with the new disease were lower.
Additionally, investigations among HCW suggest that many may have been infected within the household rather than in a health care setting. Outside of Hubei, health care worker infections have been less frequent (i.e. 246 of the total 2055 HCW cases). When exposure was investigated in these limited cases, the exposure for most was reported to have been traced back to a confirmed case in a household.
The Joint Team noted that attention to the prevention of infection in health care workers is of paramount importance in China. Surveillance among health care workers identified factors early in the outbreak that placed HCW at higher risk of infection, and this information has been used to modify policies to improve the protection of HCW.
B: Transmission in closed settings: There have been reports of COVID-19 transmission in prisons (Hubei, Shandong, and Zhejiang, China), hospitals (as above) and in a longterm living facility. The close proximity and contact among people in these settings and the potential for environmental contamination are important factors, which could amplify transmission. Transmission in these settings warrants further study.
Children
Data on individuals aged 18 years old and under suggest that there is a relatively low attack rate in this age group (2.4% of all reported cases). Within Wuhan, among testing of ILI samples, no children were positive in November and December of 2019 and in the first two weeks of January 2020. From available data, and in the absence of results from serologic studies, it is not possible to determine the extent of infection among children, what role children play in transmission, whether children are less susceptible or if they present differently clinically (i.e. generally milder presentations). The Joint Mission learned that infected children have largely been identified through contact tracing in households of adults. Of note, people interviewed by the Joint Mission Team could not recall episodes in which transmission occurred from a child to an adult.
The Symptoms
Symptoms of COVID-19 are non-specific and the disease presentation can range from no symptoms (asymptomatic) to severe pneumonia and death. As of 20 February 2020 and based on 55924 laboratory-confirmed cases, typical signs and symptoms include: fever (87.9%), dry cough (67.7%), fatigue (38.1%), sputum production (33.4%), shortness of breath (18.6%), sore throat (13.9%), headache (13.6%), myalgia or arthralgia (14.8%), chills (11.4%), nausea or vomiting (5.0%), nasal congestion (4.8%), diarrhea (3.7%), and hemoptysis (0.9%), and conjunctival congestion (0.8%).
55924 laboratory confirmed cases, typical signs and symptoms include: fever (87.9%), dry cough (67.7%), fatigue (38.1%), sputum production (33.4%), shortness of breath (18.6%), sore throat (13.9%), headache (13.6%), myalgia or arthralgia (14.8%), chills (11.4%), nausea or vomiting (5.0%), nasal congestion (4.8%), diarrhea (3.7%), and hemoptysis (0.9%), and conjunctival congestion (0.8%).
People with COVID-19 generally develop signs and symptoms, including mild respiratory symptoms and fever, on an average of 5-6 days after infection (mean incubation period 5-6 days, range 1-14 days).
Most people infected with COVID-19 virus have mild disease and recover. Approximately 80% of laboratory-confirmed patients have had mild to moderate disease, which includes non-pneumonia and pneumonia cases, 13.8% have severe disease (dyspnea, respiratory frequency =30/minute, blood oxygen saturation =93%, PaO2/FiO2 ratio <300, and/or lung
infiltrates >50% of the lung field within 24-48 hours) and 6.1% are critical (respiratory failure, septic shock, and/or multiple organ dysfunction /failure). The asymptomatic infection has been reported, but the majority of the relatively rare cases who are asymptomatic on the date of identification/report went on to develop the disease. The proportion of truly asymptomatic infections is unclear but appears to be relatively rare and does not appear to be a major driver of transmission.
Individuals at highest risk for severe disease and death include people aged over 60 years and those with underlying conditions such as hypertension, diabetes, cardiovascular disease, chronic respiratory disease and cancer. Disease in children appears to be relatively rare and mild with approximately 2.4% of the total reported cases reported amongst individuals aged under 19 years. A very small proportion of those aged under 19 years have developed severe (2.5%) or critical disease (0.2%).
As of 20 February 2114 of the 55,924 laboratory-confirmed cases have died (crude fatality ratio [CFR2] 3.8%) (note: at least some of whom were identified using a case definition that included pulmonary disease). The overall CFR varies by location and intensity of transmission (i.e. 5.8% in Wuhan vs. 0.7% in other areas in China). In China, the overall CFR was higher in the early stages of the outbreak (17.3% for cases with symptom onset from 110 January) and has reduced over time to 0.7% for patients with symptom onset after 1 February. The Joint Mission noted that the standard of care has evolved over the course of the outbreak.
Mortality increases with age, with the highest mortality among people over 80 years of age (CFR 21.9%). The CFR is higher among males compared to females (4.7% vs. 2.8%). By occupation, patients who reported being retirees had the highest CFR at 8.9%. While patients who reported no comorbid conditions had a CFR of 1.4%, patients with comorbid conditions had much higher rates: 13.2% for those with cardiovascular disease, 9.2% for diabetes, 8.4% for hypertension, 8.0% for chronic respiratory disease, and 7.6% for cancer.
The Global Response
1. The COVID-19 virus is a new pathogen that is highly contagious, can spread quickly, and must be considered capable of causing enormous health, economic and societal impacts in any setting. It is not SARS and it is not influenza. Building scenarios and strategies only on the basis of well-known pathogens risks failing to exploit all possible measures to slow transmission of the COVID-19 virus, reduce disease and save lives.
It is a new virus with its own characteristics. For example, COVID-19 transmission in children appears to be limited compared with influenza, while the clinical picture differs from SARS. Such differences, while based on limited data, may be playing a role in the apparent efficacy of rigorously applied non-pharmaceutical, public health measures to interrupt chains of human-to-pharmaceutical, public health measures to interrupt chains of human-to-human transmission in a range of settings in China.
The COVID-19 virus is unique among human coronaviruses in its combination of high transmissibility, substantial fatal outcomes in some high-risk groups, and ability to cause huge societal and economic
disruption. For planning purposes, it must be assumed that the global population is susceptible to this virus. As the animal origin of the COVID-19 virus is unknown at present, the risk of reintroduction into previously infected areas must be constantly considered.
The novel nature, and our continuously evolving understanding, of this coronavirus, demands tremendous agility in our capacity to rapidly adapt and change our readiness and response planning as has been done continually in China. This is an extraordinary feat for a country of 1.4 billion people.
2. China’s uncompromising and rigorous use of non-pharmaceutical measures to contain transmission of the COVID-19 virus in multiple settings provides vital lessons for the global response. This rather unique and unprecedented public health response in China reversed the escalating cases in both Hubei, where there has been widespread community transmission, and in the importation provinces, where family clusters appear to have driven the outbreak.
Although the timing of the outbreak in China has been relatively similar across the country, transmission chains were established in a wide diversity of settings, from mega-cities in the north and south of the country to remote communities. However, the rapid adaptation and tailoring of China’s strategy demonstrated that containment can be adapted and successfully operationalized in a wide range of settings.
China’s experience strongly supports the efficacy and effectiveness of anchoring COVID19 readiness and rapid response plans in a thorough assessment of local risks and of utilizing a differentiated risk-based containment strategy to manage the outbreak in areas with no cases vs. sporadic cases vs. clusters of cases vs. community-level transmission. Such a strategy is essential for ensuring a sustainable approach while minimizing the socio-economic impact.
3. Much of the global community is not yet ready, in mindset and materially, to implement the measures that have been employed to contain COVID-19 in China. These are the only measures that are currently proven to interrupt or minimize transmission chains in humans. Fundamental to these measures is extremely proactive surveillance to immediately detect cases, very rapid diagnosis and immediate case isolation, rigorous tracking and quarantine of close contacts, and an exceptionally high degree of population understanding and acceptance of these measures.
Achieving the high quality of implementation needed to be successful with such measures requires an unusual and unprecedented speed of decision-making by top leaders, operational thoroughness by public health systems, and engagement of society.
Given the damage that can be caused by the uncontrolled, community-level transmission of this virus, such an approach is warranted to save lives and to gain the weeks and months needed for the testing of therapeutics and vaccine development. Furthermore, as the majority of new cases outside of China are currently occurring in high and middle-income countries, a rigorous commitment to slowing transmission in such settings with non-pharmaceutical measures is vital to achieving the second line of defence to protect low-income countries that have weaker health systems and coping capacities.
The damage that can be caused by the uncontrolled, community-level transmission of this virus, such an approach is warranted to save lives and to gain the weeks and months needed for the testing of therapeutics and vaccine development. Furthermore, as the majority of new cases outside of China are currently occurring in high and middle-income countries, a rigorous commitment to slowing transmission in such settings with non-pharmaceutical measures is vital to achieving the second line of defence to protect low-income countries that have weaker health systems and coping capacities.
The time that can be gained through the full application of these measures – even if just days or weeks – can be invaluable in ultimately reducing COVID-19 illness and deaths. This is apparent in the huge increase in knowledge, approaches and even tools that have taken place in just the 7 weeks since this virus was discovered through the rapid scientific work that has been done in China.
4. The time gained by rigorously applying COVID-19 containment measures must be used more effectively to urgently enhance global readiness and rapidly develop the specific tools that are needed to ultimately stop this virus. COVID-19 is spreading with astonishing speed; COVID-19 outbreaks in any setting have very serious consequences, and there is now strong evidence that non-pharmaceutical interventions can reduce and even interrupt transmission. Concerningly, global and national preparedness planning is often ambivalent about such interventions.
However, to reduce COVID-19 illness and death, near-term readiness planning must embrace the large-scale implementation of high-quality, non-pharmaceutical public health measures.
These measures must fully incorporate immediate case detection and isolation, rigorous close contact tracing and monitoring/quarantine, and direct population/community engagement.
A huge array of COVID-19 studies, scientific research projects and product R&D efforts are ongoing in China and globally. This is essential and to be encouraged and supported. However, such a large number of projects and products needs to be prioritized. Without prioritizing, this risks compromising the concentration of attention and resources and collaboration required to cut timelines by precious weeks and months. While progress has been made, the urgency of the COVID-19 situation supports an even more ruthless prioritization of research in the areas of diagnostics, therapeutics and vaccines.
Recommendations For Uninfected Countries
1. Prepare to immediately activate the highest level of emergency response mechanisms to trigger the all-of-government and all-of society approach that is essential for early containment of a COVID-19 outbreak;
2. Rapidly test national preparedness plans in light of new knowledge on the effectiveness of non-pharmaceutical measures against COVID-19; incorporate rapid detection, large scale case isolation and respiratory support capacities, and rigorous contact tracing and management in national COVID-19 readiness and response plans and capacities;
3. Immediately enhance surveillance for COVID-19 as rapid detection is crucial to containing spread; consider testing all patients with atypical pneumonia for the COVID-19 virus, and adding testing for the virus to existing influenza surveillance systems;
4. Begin now to enforce the rigorous application of infection prevention and control measures in all healthcare facilities, especially in emergency departments and outpatient clinics, as this is where COVID-19 will enter the health system; and
5. Rapidly assess the general population’s understanding of COVID-19, adjust national health promotion materials and activities accordingly, and engage clinical champions to communicate with the media.
For the public
1. Recognize that COVID-19 is a new and concerning disease, but that outbreaks can be managed with the right response and that the vast majority of infected people will recover;
2. Begin now to adopt and rigorously practice the most important preventive measures for COVID-19 by frequent hand washing and always covering your mouth and nose when sneezing or coughing;
3. Continually update yourself on COVID-19 and its signs and symptoms (i.e. fever and dry cough), because the strategies and response activities will constantly improve as new information on this disease is accumulating every day; and
4. Be prepared to actively support a response to COVID-19 in a variety of ways, including the adoption of more stringent ‘social distancing’ practices and helping the high-risk elderly population.”















