by Imtiyaz Ahmad Bhat
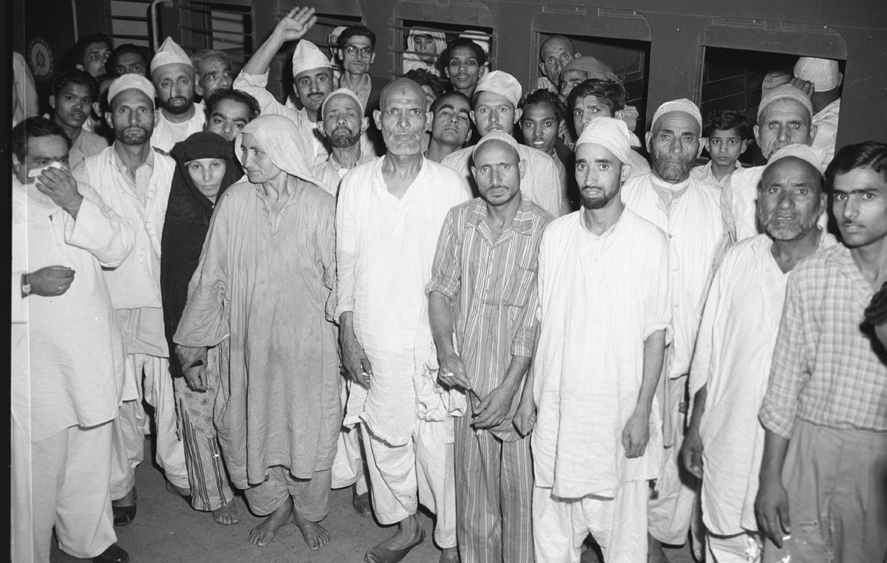
COVID-19, originated from Wuhan city of China caused by the SARS-CoV2 virus, is a potentially fatal disease that represents a major global public health concern. As per the latest reports 7 million people have been infected with around 400 thousand deaths worldwide. In India with more than three lakh positive cases and around 9000 deaths, it is turning out to be a major medical as well as economic crisis, with experts warning that the peak is yet to come.

Jammu and Kashmir has also seen a sharp spike in the number of cases from last one week with around 5000 cases and 60 deaths in total. Most of the information about COVID-19 is readily available on electronic and print media and I am not going to discuss the same here. I intend to discuss the role of diagnostics of COVID-19, its impact on the overall policy-making and different technicalities involved in the process.
During the ongoing pandemic, there is a lot of buzz regarding the possible errors in diagnosis with both RT-PCR tests and faster antibody tests, all over the world. Kashmir is not immune to such discussions. Recently a lot of hue and cry was raised in various media bulletins debating the credibility of SARS-CoV-2 testing executed by one of the testing centres in Jammu and Kashmir. The concerns raised were genuine in nature and could have been easily sorted out by randomly cross-checking 10-15% of samples from this particular lab at any other designated virology lab in Jammu and Kashmir to clear the confusion.
However, a more disappointing syndrome that has crept in our society, and which really needs a lot of attention, is that whenever an issue is raised at any social media platform, everyone tries to display his/her expertise without knowledge of the basics of the concerned subject. The consequences of such blunders were seen in 2015 when fake information regarding the vaccination of our kids was spread leading to panic and confusion among the public. During the recent wave of chaos and confusion amidst the general public, I was called by many friends who were deeply concerned about the authenticity of SARS-CoV-2 testing procedures. It was then I realized the need to educate the common people about the SARS-CoV-2 testing. Therefore, I am utilizing this opportunity to explain some basics of SARS-CoV-2 testing and the various technical reasons that could lead to either false-positive or false-negative results.

The first and foremost thing that we need to understand is the fact that if a new testing facility is rapidly developed and deployed, the accuracy cannot be predicted beforehand. A test developed under controlled laboratory conditions might behave in a different way when applied in the real world and this might enhance the likelihood of errors due to many unforeseen events.
In all probabilities four types of outcomes can occur during any diagnostic test: True positive, False Positive, False-negative and True negative, with True Positive and True negative being the desirable outcomes for any lab, while as False-negative and False positive are the errors which every testing centre would try to minimize. Usually, every diagnostic procedure is designed to achieve 100% sensitivity and specificity, but despite the best efforts, Kassirer’s statement “No diagnostic test can be 100% accurate” always holds true.
So whenever a result comes out to be negative (or positive), there still is always some probability of having (or not having) a disease like COVID-19 due to the inherent possibility of errors. Antibody testing is cheap and easy to perform in comparison to RT PCR and holds significant importance in community screening to trace the development of antibodies (herd Immunity) but the same can’t be termed as an alternative to diagnostics of SARS-CoV-2 virus.
With this background, I would like to discuss some of the basics of RT PCR diagnostics for SARS-CoV-2 and my own experiences while working on the same in one of Kashmir’s diagnostics centres. As per the WHO guidelines both the symptomatic patients and the asymptomatic carriers (mild, pre-symptomatic and asymptomatic) need to be screened for Coronavirus 19. An asymptomatic laboratory-confirmed case is a person infected with SARS-CoV-2 who does not develop symptoms and his/her screening is of vital importance to stop the transmission of the virus in a community.
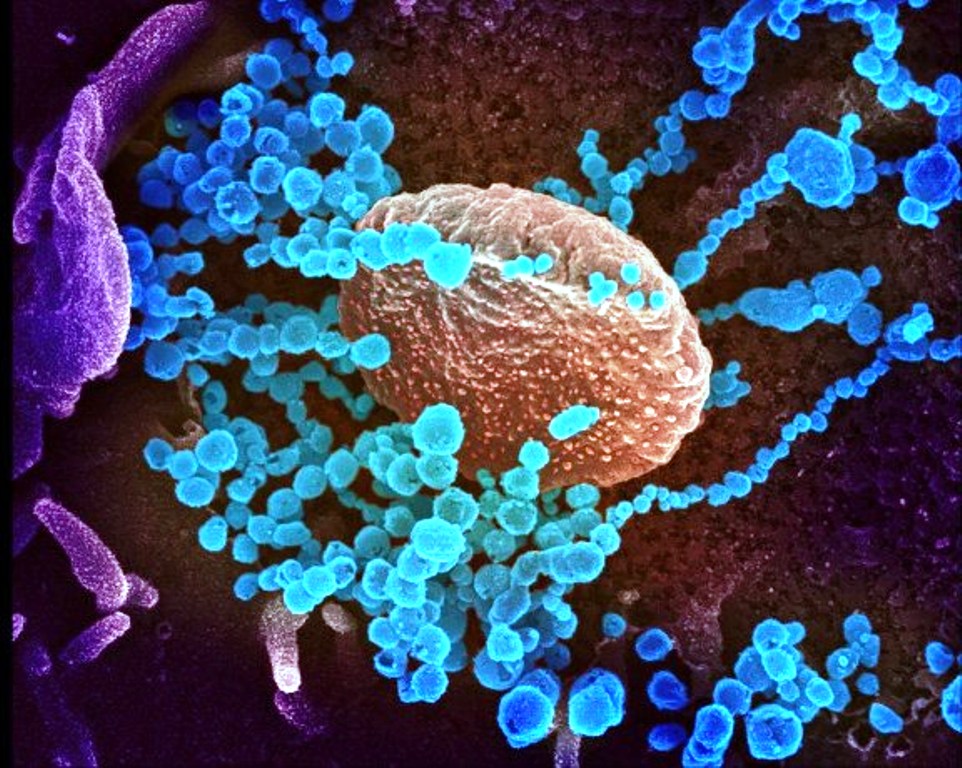
SARS-CoV-2 diagnostics is performed by amplifying the genomic material by Real-Time Polymerase Chain Reaction (RT-PCR). The results thus obtained are used to diagnose and determine the treatment of patients, quarantine individuals, guide contact tracing and to allocate the use of personal protective equipment. At the policy level, test results are used to model rates of spread, calculate hospitalization and death rates, assess the number and significance of asymptomatic carriers, shape up public policy on social distancing, and in decision making about the spatial and temporal allocation of medical resources. The test accuracy is thus of paramount importance, yet little attention has been paid to the potential frequency and impacts of false-positive and false-negative results.

Although SARS-CoV-2 RT-PCR assays are widely reported to have 100% specificity, this is based on the assumption of absence of cross-reactivity with non-target genetic material (analytical specificity), and not to the potential for incorrect results in the real-world implementation of testing (clinical specificity) wherein contamination or human error can generate false positives during sample collection, transport or analysis. Researchers have also found that testing people for SARS-CoV-2 too early is likely to produce false-negative results which are very dangerous in nature as it places the lives of others at risk when we assume the test is perfect.
The researchers at the John Hopkins University estimated that people tested with SARS-CoV-2 in the first four days after infection were 67% more likely to test negative, even if they had the virus. When the average patient began displaying symptoms, the false-negative rate was 38% and the test performed best after eight days of infection but even then had a false negative rate of 20%.
The various steps and technicalities of SARS-CoV-2 testing by RT PCR and the possibilities of false-positive results due to various lab errors are further described here for general awareness. However, we first need to understand two major causes that can lead to false results.
The first step is Sample Sorting and Sample Pooling. Once the sample (nasopharyngeal or buccal swab) is collected and transferred to the lab in stringent cold conditions. The samples are sorted and given proper lab IDs for further processing. During pandemics, samples are pooled meaning 5-10 samples are mixed together to form one pool for analysis. This strategy is not routinely performed for diagnostics, however, under limited resource settings of pandemics, the method is followed for increasing the testing capacity of our labs. Sample pooling for SARS-CoV-2 testing is recommended by ICMR and other medical agencies to avoid the cost and enhance the testing rate.
After the extraction of RNA and RT PCR completion, if any of the pool of samples turns out to be positive, then all the samples are processed individually for RT PCR. The pooling of samples does not affect the quality of testing in case of amplification assays as even a single strand of RNA is enough to be picked by the RT PCR thus diminishing the chances of false-negative results. However, other reasons for false-negative results as described earlier cannot be ignored. Extra caution is taken during pooling of samples to avoid any chance of cross over contamination of samples. Trained and responsible staff with enough expertise in pipetting and handling of infectious samples, is usually assigned for this job since small negligence at this juncture can spoil the whole testing procedure.
The second step includes extraction of genomic material for amplification and to detect the presence of SARS-CoV-2. This second most important step in any PCR based diagnostics includes extraction of genomic material of the infectious micro-organisms. The extraction of nucleic acid material is nowadays performed by the nucleic acid extraction kits supplied by various companies.
The introduction of extraction kits for nucleic acid extraction is based on the principle of selective binding property of silica-based membranes, which are highly specific for nucleic acid material followed by centrifugation. This step is very short and takes about an hour or so for completion. The extraction of nucleic acid material usually done by extraction kits looks very simple but this is the step where most of the errors can creep in. The possibility of carry-over contamination is very high as the generation of aerosols in the extraction area can lead to cross-contamination of the samples.

The third and the most vital step is RT PCR and Data Analysis for the detection of SARS-CoV-2. The principle of RT PCR includes using special fluorescent probes and primers designed against different genes (E, ORF, N, S etc) which are unique to SARS-CoV-2 and the use of Non-template control, negative control and positive control for its detection followed by data analysis.
If the sample is infected with Coronavirus, the fluorescent probes and primers will bind to the extracted nucleic acid targets, followed by the release of fluorescent emission which is captured by the RT PCR and interpreted in the form of CT values and amplification plot. The setting of RT PCR is usually carried out in the laminar hood located away from the extraction area to avoid any carryover contamination. The most common errors that can occur during the analysis of the Real-Time results can be due to the use of low standard reagents and equipment’s not approved by US FDA, poor understanding of the data analysis in RT PCR like directly interpreting the CT values without their correlation with the amplification plot, not using of controls (NTC, negative and positive controls).

In normal circumstances in RT PCR assays, every sample is run in triplicates to avoid any errors but the same is not possible due to the shortage of reagents and a huge rush of samples in pandemic situations like SARS-CoV-2, but still, as a compensation measure at least 05% of the samples are cross-checked at other centres to avoid any False reporting. The impact of False-positive and False-negative in SARS-CoV-2 testing could be mitigated by increasing and improving awareness of the probability of false positives and false negative; by improving estimates of false-positive and negative rates with appropriately-designed external quality assessments, or assessing results retrospectively with serological tests; and by reducing the frequency of false-positive and false-negative by requiring two independent tests to classify an individual as positive or negative.
Tail Piece
With all these diverse complexities associated with molecular SARS-CoV-2 testing, I would request the administrative officials and the health officials as well, to kindly ensure that only the expert microbiology and molecular biology professionals are handling this testing process and the process of temporary deployment of professionals for short durations should be abolished, so that we may achieve the international standards of SARS-CoV-2 testing.
(A master in biotechnology, Imtiyaz Ahmad Bhat has PhD in Immunology and molecular medicine. Currently, he is a researcher and senior resident in the Department of Immunology and Molecular medicine, SKIMS. The opinions expressed in this article are those of the author’s and do not purport to reflect the opinions or views of Kashmir Life.)