by Dr Kouser Sideeq
The term herd immunity includes two words. Firstly, the herd which originated from a German word heord, means a large group of people or animals. The other word immunity means protection. Thus the term literary means group protection. Regarding infectious diseases, the term herd immunity has been described with a variety of meanings.
Some researchers use it to describe the proportion of immune among individuals in a population. Others use it with reference to a particular threshold proportion of immune individuals that is required to decline the incidence of a particular infection. Herd immunity also refers to a pattern of immunity that should protect a population from the invasion of a new infection. Overall, what is derived from all common implications of the term is that the risk of infection among susceptible individuals in a population is reduced by the presence and proximity of immune individuals this phenomenon is called as ‘herd effect’’.
Evolution
Herd Immunity was not widely used until recent decades. Its use was stimulated by the increasing use of vaccines, disease eradication processes, and for the costs and benefits analysis of vaccination programs. An individual’s immunity can be acquired via natural infection or through artificial means, such as vaccination. It was in the 1930s when herd immunity was first recognized as a naturally occurring phenomenon by A W Hedrich, in his research on the epidemiology of measles in Baltimore. He took notice that after many children had become immune to measles, the number of new infections temporarily decreased, including among susceptible children. In spite of this knowledge, efforts to control and eliminate measles were unsuccessful until the measles vaccine came into use in the 1960s.
In 1970s Smith and Dietz gave a theorem to calculate a disease herd immunity threshold for vaccination. The theorem says that —that if individual members of the population become immune at random (due to vaccination) to the proportion that exceeds R0-1 or 1-1/ R0 then the incidence of the infection would decline. Here R0 denotes the number of individuals who would be infected on an average due to contact with each infected individual and is called a basic reproduction number.
Using this theorem it was established that when a critical proportion of the population becomes immune, called the herd immunity threshold (HIT), the disease may no longer persist in the population, ceasing to be endemic. Individuals who are immune to a disease act as a barrier in the spread of disease. Many theories and formulas have been developed to derive R0 for different infections, implying that the 1 – 1/R0 threshold be used as a target for immunization coverage and that its achievement can lead to the eradication of particular target infections.
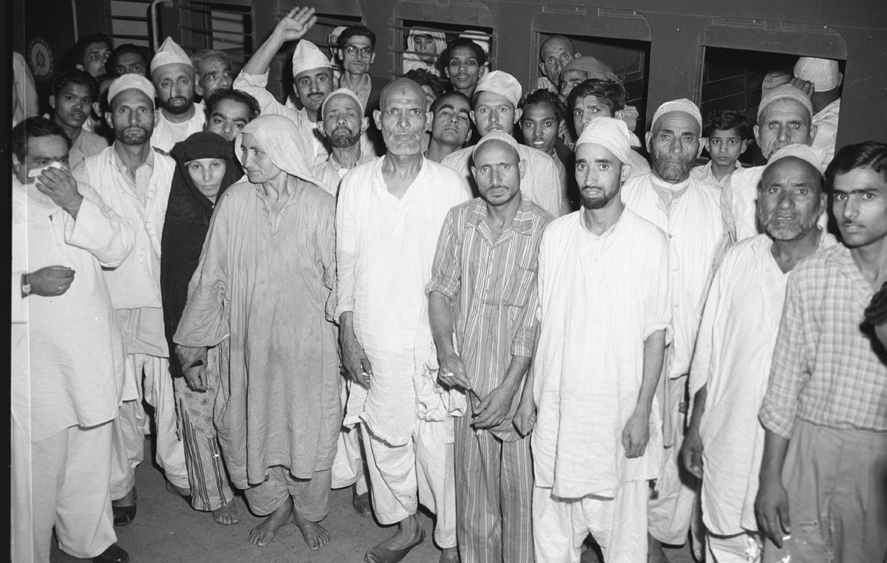
During the smallpox eradication campaign in the 1960s and 1970s, the practice of ring immunization, of which herd immunity is integral to, began as a way to immunize every person in a ring around an infected individual to prevent infection from spreading. These all concepts of herd immunity due to vaccination also apply to the immunity conferred to individuals due to recovery from certain infection when vaccination is not available.
Herd Immunity And Covid-19
All over the world most of the countries adopted the containment strategy to stop the spread of this disease, from closing schools and universities to locking down entire countries. For the development of herd immunity, an alternative strategy would have been to allow the virus (SARS-CoV-2) to spread, while at the same time protecting the groups like elderly and those with multiple co-morbidities, who are the most vulnerable to this virus.
For initiating any of the strategies we need to estimate the basic reproductive number (R0), or the effective reproductive number (Rt) for a given population. As already said R0 is the number of secondary cases generated by the presence of one infected individual in an otherwise fully susceptible, well-mixed population. Rt is a more practical real-life version of this, which uses real data to estimate the reproductive number for an epidemic. Rt for the Coronavirus diseases has been calculated using different mathematical software and in the majority of countries including India, it is between 2 -4.
Using these values of Rt, we can then calculate the minimum (critical) level of population immunity (Pcrit) acquired via vaccination or naturally-induced (i.e. after recovery from COVID-19), to halt the spread of infection in that population, using the formula: Pcrit= 1-(1/Rt). So, for example, if the value of Rt = 4 then Pcrit= 0.75, i.e. 75% of the population need to be immune.
Majority of the countries would need to have the proportion of the population which becomes immune due to recovery from Covid-19 to be equal to around 65 -75%.
Looking at the current evidence of herd immunity for Covid-19 few studies have established positive developments.

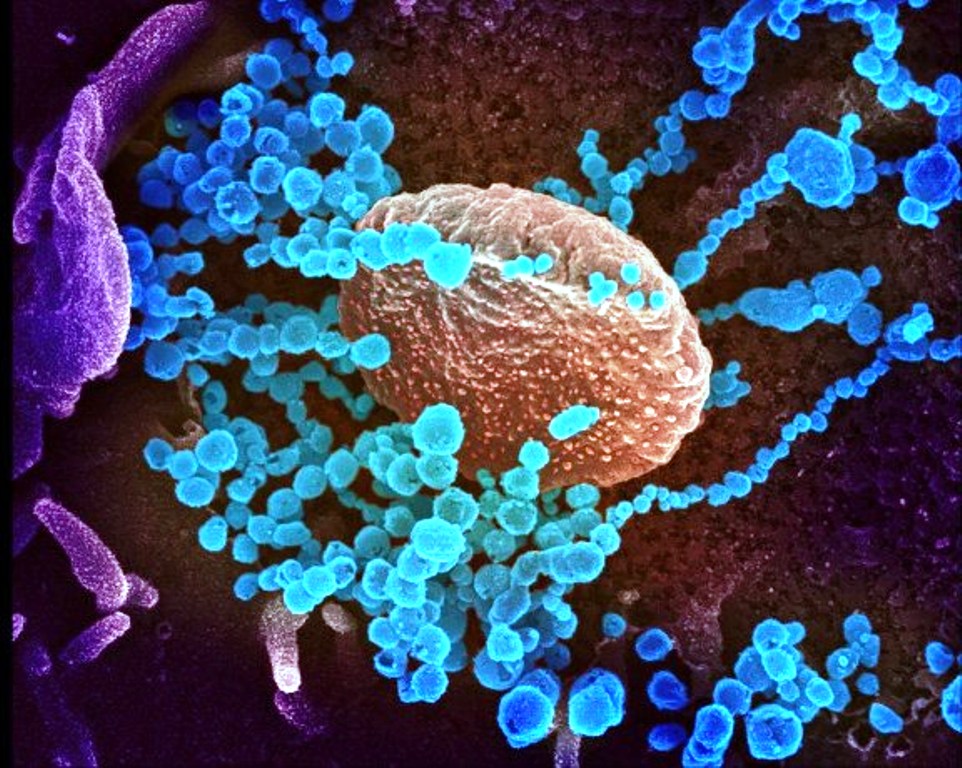
A population genetic study was conducted by Tang X, Wu C, Li X, et al on the origin and continuing evolution of SARS-CoV-2. They studied 103 SARS-CoV-2 genomes and identified two viral subtypes of SARS-CoV-2 designated as S and L types. Further research found that the epidemic seemed to be subsiding in areas where S type virus was predominant. Such results prompted researchers to hypothesize that the infection by S type induced herd immunity that provides at least partial protection against the spread of SARS-CoV-2.
Researchers in Japan further suggested, that spread of S type before the L type coronavirus confers partial herd immunity to the L type also. The case fatality rate (CFR) of Covid-19 has been between 0.25–3.0% in the majority of countries and being even more in some countries. The estimated number of people, who could potentially die from Covid-19, whilst the population reaches the Pcrit (threshold) herd immunity level, may be difficult to accept for the countries but if the vaccine is discovered soon then that will be the breakthrough to establish herd immunity without the risk of mortality.
The development of herd immunity due to infection cannot be part of the action plan to tackle coronavirus, but it is a natural by-product of an epidemic. As rightly said by NHS (National Health Service England), “Herd immunity is a scientific concept, not a goal or a strategy.” Many of the important things related to the current Coronavirus pandemic is not known yet, and the most important thing regarding the development of herd immunity is that it is not clear that how long those who are infected are subsequently immune for. Some other viruses in the Coronavirus family, such as those that cause the common cold, only provide immunity for around three months approximately.
Scientists have found that there’s evidence for short-term immunity [after contracting Covid-19], but there is no data yet to know whether it provides long-term immunity or not. Dr Jeremy Rossman, Honorary Senior Lecturer in Virology at the University of Kent estimates that we’d need to be immune to the coronavirus for at least a year, possibly two, in order for the population to build up herd immunity. Otherwise, our best hope for herd immunity might be a vaccine which is still under trials and can take much time. There’s a chance that we could control the epidemic before we need the full protection of herd immunity taking China as an example.
Another important thing that is still under investigation for SARS-CoV-2 is that how much this virus will mutate over time. The viruses that cause flu are constantly mutating, which is why people need annual vaccinations to protect against the most prevalent strains that year.
Current world faces the challenge of controlling this pandemic, with various strategies of lockdown and hope for the vaccine meanwhile the spread is continuing and herd immunity may take its natural course to finally cease it to be an endemic disease. Measures can be taken to make it harder for a disease to spread (reducing the value of R0), and this, in turn, reduces the herd immunity threshold.
(The author is Assistant Professor Department of Community Medicine, Govt Medical College Baramulla)