by Jaibeer Ahmad
Imagine every day the attendant has to narrate the whole history of the patient to a new doctor in less than two minutes

A friend once told me that she would prefer to die in her home without any treatment than getting hospitalised. I got the import of her words when my grandmother had to be hospitalised a month back.
Yes, it is nothing less than a curse to be hospitalised in Kashmir. I will deliberately refrain from naming the hospital as it is not one particular facility that is mismanaged; it is the system, the culture that is in a deplorable state. The experience for anyone across hospitals in Kashmir would be no different than mine.
My ordeal started about four weeks back when she was admitted in the emergency unit of a district-level hospital for a blood infection and suspected pneumonia (non-Covid19). She had to be brought to the hospital very early in the morning, in a serious condition. At that time the reaction of the junior doctors and the paramedic staff on the night duty was prompt, they lost no time in starting the treatment and making us aware of her critical status. They were on their toes and despite being overworked they were exceptionally good.
An End To Good Story
Sadly, except for a few more professional and humane gestures we encountered later on, that is where the good side of the story nearly ends.
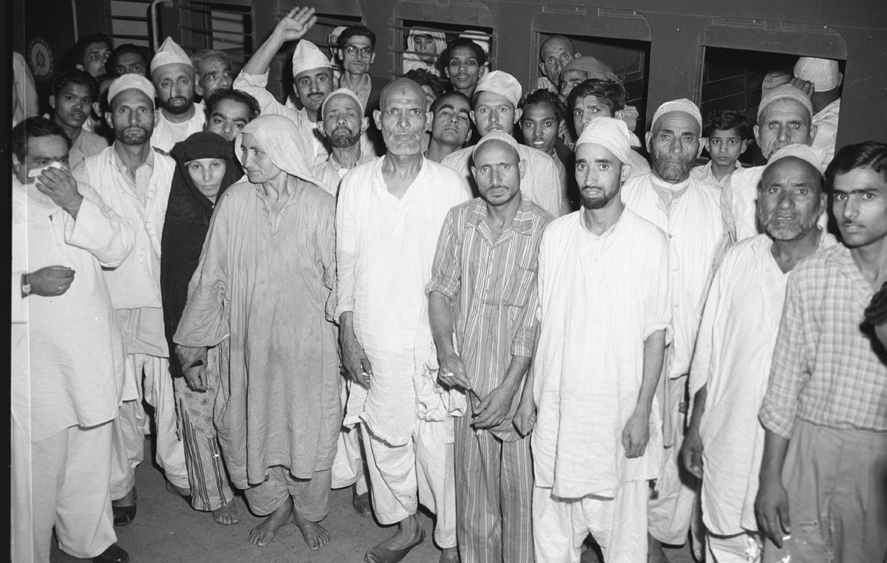
The emergency or the casualty section, if you have been unfortunate to had to visit one, is like an overcrowded, dirty and chaotic street. You are lucky if you get a bed to yourself. Many patients end up sharing beds or on stretchers converted into make-shift beds in the corridors. This is true for non-covid times as well. We were lucky enough to get a bed in a small trauma room. But soon I realised the place is ill-equipped as we couldn’t get an X-Ray done because there was no portable machine available. Later, I noticed it was not even possible to get one into the ward, there is no space for a portable machine to be moved around.

However, the real horror started the next day when we realised a seriously sick Covid19 patient was admitted on the next bed, just 2 feet away from my grandmother who lay fully exposed without any mask (By this time one had understood that social distancing is just a privilege, which doesn’t count here). As soon as we got to know about the patient bring Covid19 positive, we started panicking and requested everyone around to shift her to a Covid19 ward, only to be told there were no beds available. More than the fact that there was no segregation of Covid19 and Non-Covid19 patients it was the casual attitude that was shocking. The Covid19 patient, an elderly lady lay there on oxygen support for next several hours. Nevertheless, we kept trying and only in the evening around 8pm the patient was shifted to a Covid19 ward. We barely had a sigh of relief when another Covid19 patient landed on the same bed on the same night.
By now we were convinced that we needed to shift the grandmother out of the emergency unit to a ward where there were fewer chances of Covid19 patients getting mixed up.
All For A Bed
But getting a bed in a ward was not going to be easy, a bed needed to be occupied physically. You have to find one on your own. That is the simple rule. There is no system of allocating one. After spending half a day looking for one without much luck, a sympathetic hospital employee helped me locate a bed. He left me with the advice that I do not leave it unoccupied till the patient was shifted. It was a real estate that needed to be grabbed and guarded.
Sure enough, I had to fight off a few other attendants who were looking for beds for their patients till we managed to shift her in, after begging for an oxygen cylinder from multiple people.

Breathing a sigh of relief, we thought now things would get better. The ward was more spacious and cleaner than the emergency unit. But here also, given an abysmal paramedic staff ratio, almost everything has to be managed by the family and the attendants. From getting food for the patient to changing the bedsheets to fetching the doctors or the nurses to getting tests done everything had to be done by the attendants.
For a simple blood test it is the attendant who has to first get a vial issued after making a payment, then get the blood sample and deposit and the lab and later on get the results. If it is a test like an ECG done you have to beg, plead or shout to get the technicians to agree to do it.
There are many patients with a single attendant who have to request others to help them manage. Some patients come from far off places and struggle for basics. A man from a far off village had converted his old car into a kitchen and bedroom in the parking lot.
On the way, you do meet some good humane people like a lab assistant or a nursing orderly who will go out of the way to help you. You also meet some callous ones like an ICU assistant who refused to help take a blood sample despite a written request by a doctor, or an ICU in charge who would get an ultrasound done despite a portable machine available to him.
Diversity Of Doctors
However, the bigger and more worrisome problem is not these hassles. It is the doctor and the process and ethics of treating patients. Every day a senior doctor or a consultant takes a round of the ward to review the patients. But the problem is that it is a different doctor every day!
In a week there were five or six different doctors who see the patient. Each one spends about 5-10 minutes with the patient which in any circumstances is not enough for any doctor to know the history of the patient, make a good assessment, especially in serious cases. They tend to follow the previous day assessment and the same diagnosis continues. No one owns the patient.
Imagine every day the attendant has to narrate the whole history of the patient to a new doctor in less than two minutes. There are other problems too, for example, twice in our case they also missed prescribing medicine, which if not highlighted by the attendant would have proved serious for my grandmother. The other challenge is the inaccessibility of senior doctors. Post the round of the ward, the senior doctors are rarely available. There is no way to contact them even in case of an emergency, no phone numbers left behind. It is only left to the junior doctors who have to manage even in serious situations. I found a majority of the junior doctors to be diligent and sincere and more sympathetic.
To ICU
After about two weeks, my grandmother’s condition deteriorated further and the doctors advised her to be shifted to the ICU. She had to be on high flow oxygen. But getting an ICU bed wasn’t going to easy either. It took some lobbying and multiple requests to get one. The ICU expectedly is better equipped, the nurses maintain a proper chart for the medication and reports. But beyond that again everything else has to be managed on your own.
One of the peculiar things that I noticed is that the nursing staff also goes off to sleep at night. You have to wake them in case of any help needed. Once when I did the same in an emergency I was rebuked by the nurse for knocking persistently on her “bedroom” door.

Working nights is seemingly an enormous challenge. For instance, the storekeepers leave at 4 pm. In the ICU on day 1, we had to struggle for a spare bed sheet because the storekeeper’s duty was over.
On the second night, the high-pressure oxygen pipe leaked. A spare one was removed from another machine, which again leaked. In the meantime, my grandmother’s oxygen level dropped to 50. Luckily someone fixed the pipe on time and saved her. There was no way to get a spare pipe as the stores were long shut. On the third night, the machine stopped working altogether.
The Committed Staff
At this point, I would want to highlight the commitment and efforts of the lower end staff. The sanitation workers and the guards specifically are way ahead in terms of their professionalism and dedication. They leave no stone unturned in doing their duties but are defeated by the callous behaviour and attitude of the people.
It is disdainful how we treat the facilities. The condition of the washrooms, for instance, is pathetic. It is not because of lack of cleaning but because of how we litter, throw garbage in latrines, mishandle the utilities and general attitude towards cleanliness. The guards have a difficult time too keeping the relatives out of the wards. Where there are one or two attendants needed an army of relatives keeps pouring in. At times there are 8-10 people surrounding a patient, putting an enormous burden on the system as well as risking the lives of the admitted patients.
My grandmother passed away after struggling for her life for three weeks in the hospital.
Not A Rant
I am aware that my experience is not as bad or tragic as so many others that we keep reading about. There are far worse experiences and I dread to imagine what it would be like in smaller hospitals and with poorer less literate patients.
I am also aware that this piece will probably never reach the corridors of power that possibly could change some things. Those who will come across it most will probably dismiss it as yet another rant, many will curse the system and some will feel as helpless as I do.
The truth is, I will also move on.

The truth also is that the system needs to be shaken, the behaviour of people needs to change, the truth also is that unless we will also need to contribute to the hospitals through donations, charity and voluntary service to make it better. A lot more charity can be diverted to the hospitals; it will reach the needy and the poor. A lot of services are medicines are provided free at the hospital. There are patients whose families can afford these. Maybe they can contribute back by donating some money and equipment to the hospitals.
Despite the hopelessness, I felt in the last one month, small steps of change, I feel can go a long way
(The author works as a Senior Vice President with a multinational advertising agency in Gurgaon. He was behind the JK Tourism Campaign Warmest Place on Earth and Raabta, an initiative to bring Kashmiri Pandits and Muslims together.)